Abstract
Introduction: Patients with myelodysplastic syndromes (MDS) who present with isolated thrombocytopenia (TP) represent an infrequent group. Previous studies have described clinical presentation and outcomes but none of them include the gene mutation profile. The aim of the present study was to define molecular profile and overall survival (OS) in patients with MDS-TP.
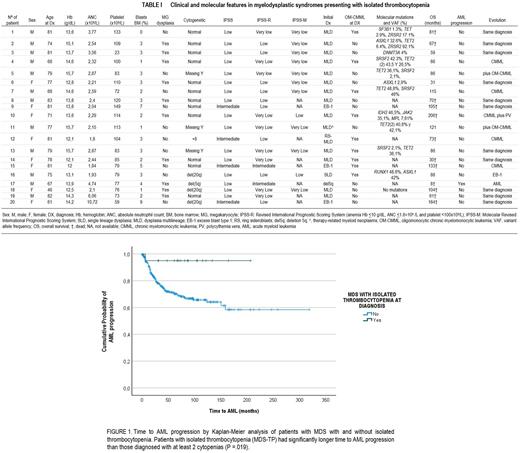
Methods: We retrospectively studied 472 patients diagnosed with MDS between Sep/1988-Jun/2022. Diagnostics were established according to WHO 2017 criteria, and prognosis assessment according to IPSS-R and IPSS-M. MDS-TP patients were defined by: Hb ≥12 g/dL (female) or ≥13 g/dL (male); absolute neutrophil count ≥1.8×109/L and platelet <150x109/L. NGS sequencing data were available in 12 patients. We analyzed the full exonic regions of 25 genes associated with myeloid neoplasms (ASXL1, CALR, CBL, CSF3R, DNMT3A, ETV6, EZH2, IDH1, IDH2, JAK2, KIT, KRAS, MPL, NRAS, PRPF8, RUNX1, SETBP1, SF3B1, SH2B3, SRSF2, STAG2, TET2, TP53, U2AF1, and ZRSR2).
Statistical analysis: Categorical variables are described by frequencies and percentages and continuous variables as medians and ranges. Survival curves were constructed by the Kaplan Meier method, defining OS as the interval from date of diagnosis to last contact or death, and time to AML progression as the interval from date of diagnosis to AML progression. Survival curves were compared by log-rank test. We performed a cox regression analysis for adjusting the prognostic impact of MDS-TP by IPSS instead of IPSS-R since the latter contains thrombocytopenia as a prognostic variable. Differences were considered statistically significant when P<.05 in a 2-tailed test.
Results: Of the 472 patients meeting MDS criteria, 20 (4%) had MDS-TP. Median age at diagnosis was 74 years (46-83). Median platelet was 84x109/L (23-149). Median follow-up was 83 months (8-200). Median OS was 104 months (68-206). None of the patients required treatment at diagnosis. Twelve (60%) patients died during follow-up, 4 (34%) due to infections, 2 (16%) to arrythmia, 2 (16%) solid cancers and, 1 (8%) to AML. The distribution according to WHO was: 14 (70%) MDS with multilineage dysplasia (MLD), 3 (15%) MDS with excess blasts type 1, 1 (5%) MDS with single lineage dysplasia, 1 (5%) MDS ring sideroblasts with MLD, and 1 (5%) MDS 5q deletion. Twelve (60%) had normal karyotype, 3 (15%) chromosome Y loss, 3 (15%) 20q deletion, 1 (5%) chromosome 8 gain and 1 (5%) 5q deletion. No complex karyotype was observed. IPSS-R distribution at diagnosis was: 45% very low, 45% low, and 10% intermediate. According to IPSS-M, 10/12 (83%) were very low and 2/12 (17%) low. The most common mutations were: 6 (30%) TET2, 3 (15%) SRSF2, 3 (15%) ASXL1, and 2 (10%) ZRSR2; 2/6 patients with TET2 mutation had 2 TET2 mutations. One patient did not present any mutation. Nine (45%) patients met oligomonocytic chronic myelomonocytic leukemia (OM-CMML) criteria at diagnosis, and 2 of them during follow up. Five (25%) patients evolved to CMML. Half of the patients did not present megakaryocytic dysplasia, regardless of WHO category. Interestingly, 4 patients diagnosed with MDS-MLD, which also met OM-CMML criteria, improved thrombocytopenia after short-term steroid use due to not related purposes (i.e: SARS CoV2 infection). OS was significantly longer in MDS-TP (median OS, 104 vs 48 months; p=0.036). Time to AML was also significantly longer (p=0.019). Figure 1. When adjusted by IPSS, MDS-TP did not remain as an independent good prognostic factor but showed a clear statistical trend for both OS (p=0.08) and time to AML (p=0.06).
Conclusions: We found MDS-TP to be more frequently associated with MDS-MLD, normal karyotype and lower IPSS-M and IPPS-R. Most common mutations were TET2 and SRSF2, similar to OM-CMML and CMML. In this regard, almost 50% of patients met OM-CMML criteria at diagnosis or during follow up and 25% evolved to CMML. We hypothesize that isolated thrombocytopenia as the sole cytopenia at diagnosis of MDS would probably be linked to autoimmune phenomena at least in a higher proportion of patients. In this line, half of the patients did not present megakaryocytic dysplasia, some of them improved their thrombocytopenia with steroids, and the series is enriched in TET2 mutations, that have been linked to autoimmune phenomena in several articles (eg: Zhao LP et al. Leukemia 2021). Finally, this group of patients showed a significantly better OS and time to AML.
Disclosures
Salar:BMS/Celgene: Honoraria; Beigene: Honoraria; Roche: Research Funding, Speakers Bureau; Abbvie: Research Funding; Incyte: Speakers Bureau; Gilead: Research Funding; Janssen: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal